Amylin, Insulin Resistance and Brain Health
- Bowie Matteson
- Aug 15, 2023
- 4 min read
Insulin resistance is our body's inability to utilize insulin, a critical peptide in our body's utilization of glucose as cellular energy. After we eat, insulin, secreted by beta cells of the pancreas, is responsible for sequestering the glucose molecules being circulated in our blood into each and every cell in order for that glucose to be used for energy.
When we chew our food there is an elaborate cascade of preparatory secretions and alignments that allow for our food to be properly handled and circulated. Stomach acid starts to be released as soon as our tongues detect the composition of our meal, the sweet sugar molecules, the rich, savory fat molecules, the hardy proteins and litany of micronutrients.
Insulin and amylin, both of the beta cells, are similarly released by the pancreas to help assimilate the food we've eaten into our system:
Insulin for getting the glucose into our cells
Amylin for pacing digestion, promoting feelings of fullness and thus aiding insulin's efficiency and ability to maintain blood sugar homeostasis
Insulin, thus far, has stolen the show in terms of popularity. With diabetes reaching epidemic proportions globally, insulin and secondary measures of optimizing its release and absorption have become a top priority in the modern healthscape.
Amylin, on the other hand, has remained mysteriously under the radar. I would go so far as to say the great majority of diabetics know nothing about it. I know I didn't. As someone who has had type 1 diabetes since 2001, I didn't know it existed until about 2 months ago.
Why is that?
Amylin's omission in our healthcare system is a byproduct of the continued uncertainty and ambivalence surrounding the 12-headed monster of chronic inflammation and insulin resistance. Modern research has failed to consolidate any singular source of our inflammatory woes. To be a consumer in the market of healthcare options is a confusing place to be. Many theories and tangential attempts at addressing symptoms seemingly point in opposing directions. Low carb, high fat? Fat is bad, protein is better? Take your meds, but not too much or else you'll develop a new condition. Be wary of vegetables, meats and anything in between.
In this sea of symptom management, the collective we (professionals and general population alike) have lost our way in understanding what we're actually after. We've abandoned our duty to continually reevaluate our understandings of our condition in order to find the next "big thing" that's going to make us feel better right now.
Amylin is a victim of that symptom management obsession. But it's been avoided long enough and has begun to rear its head in the form of degenerative mental disorders, like dementia and Alzheimer's disease (AD).
Amylin is co-secreted with insulin. As insulin goes up in our system, so does amylin. In our obsession with the fluctuations of insulin in an inflammatory state, we've taken amylin for granted.
In states of insulin resistance, there is an overabundance of insulin in circulation. The loss of cellular sensitivity to insulin causes our beta cells to produce more in order to reach the desired effect. But remember: more insulin, more amylin.
The effects of excess insulin (or hyperinsulinemia) have been well-documented. But what about amylin? If there's too much insulin in circulation, that means theres too much amylin too.
As it turns out, amylin, when in excess, likes to clump together, or aggregate. Amylin aggregation has become a known risk factor in the development of neurodegenerative plaques.
A simple Google search on "amylin and Alzheimer's disease" will turn up plenty of papers mentioning Amyloid-beta plaques, islet amyloid polypeptide and dementia. Islet amlyoid polypeptide (IAPP) is another word for amylin. They are the same thing.
The term amyloid-beta describe any number of amyloid beta proteins of similar size and shape that exhibit several regulatory and protective measures in a healthy system.
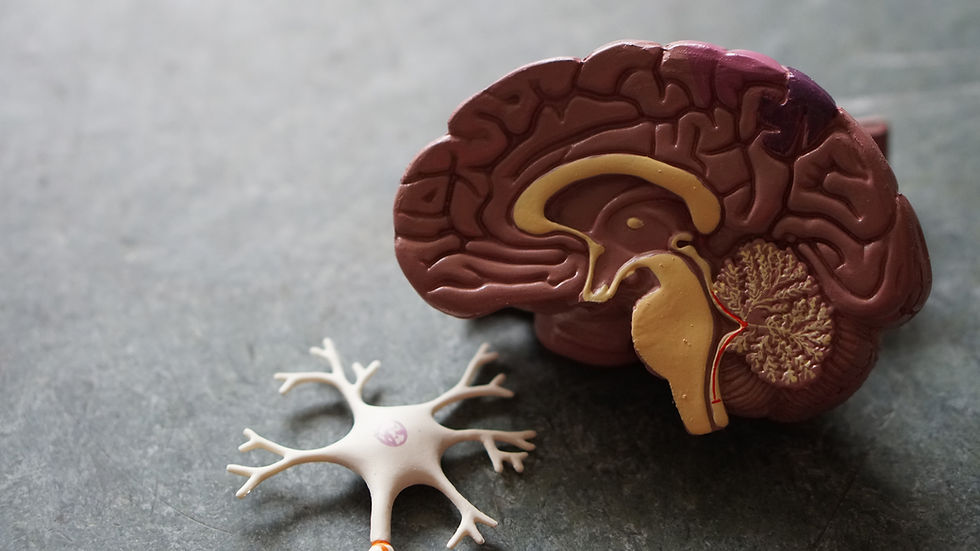
While their true origins and purpose remain somewhat unclear, amyloid beta proteins have an undeniable role in the development of neurodegenerative diseases. The clumps of amyloid proteins tend to form cohesive sheets that accumulate in between and around neurons. Amyloid-beta plaques isolated from the brains of patients with AD have been found to limit the brain's natural synaptic plasticity and memory formation.
Think of it like shrink-wrap suffocating brain cells and preventing them from communicating with one another.
These aggregates promote misfolding of proteins, disrupt cellular membranes and prevent proper cell function. The effects of this cascade are not isolated to the brain, either. In diabetics, amylin aggregation has been listed as having a potential role in beta cell death and dysfunction as well.
So, as you can see, there is an intimate link between augmented insulin levels, the resulting amylin levels and the ensuing amylin aggregation leading to harmful plaques effecting the human brain.
Its anyone's guess at this point exactly how insulin resistance is started. In my own research and self-experimentation, I've isolated nutrient deficiencies and mineral imbalances as the cracks in the proverbial foundation from which all our inflammatory woes are built.
Iron, a reactive pro-oxidant typically reserved for catalyzing energetic exchanges in our body, has risen to the top of my list of things to take care of. Iron is unique in its relation to mitochondrial health, glucose metabolism and insulin secretion. It delivers oxygen to our cells via hemoglobin in the blood. It exists as an electron acceptor/donor in the electron transport chain of cellular respiration. With its ties to metabolism and cellular energy, it has an intimate relationship with the proteins and hormones responsible for facilitating energy uptake and delivery. Hormones like INSULIN.
Given the unregulated, hyper-processed and artificially fortified nature of much modern food stuffs, our bodies' natural balance of vitamins, minerals and micronutrients has been skewed so far away from any healthy order that we are beginning to implode upon ourselves. Everything about iron and the pathology of its mishandling paints it as a kingpin. I've written about this extensively and host a podcast on the matter.
So might addressing nutrient imbalances and mineral deficiencies target the root cause of inflammation?
Might a focus on restoring balance to simple, affordable and accessible minerals heal the deep-seated wounds of our metabolism?
With a rebalanced system, might our insulin sensitivity return, our insulin and amylin levels normalize and our inflammation subside?
It certainly seems possible.



Comments