Imunofan: Immunomodulatory Peptide and Potential Role in Type 1 Diabetes
- Bowie Matteson
- Mar 30, 2025
- 46 min read
If you've been an active consumer in the world of holistic wellness and alternative medicine chances are that you are familiar with peptides. These artificially enhanced short amino acid sequences are designed as mini proteins for targeted biological outcomes. Things like BPC-157 and TB-500 are very popular now in the mainstream alternative health world for their pharmaceutical level efficacy without the pharmaceutical level side effects.
Perhaps more popular in the realm of sports medicine for performance enhancing benefits, peptides have been operating in the shadows of pharmaceutical advancement for several decades. I remember taking BPC-157 during my intense fascination with weightlifting and training. Body protective compound is marketed to help your body heal faster after acute tissue damage, whether that be recovering from an injury or promoting new tissue and vascularization after training sessions.
In the realm of diabetes research (and western clinical practice in general), peptides are less prevalent. However, when you take a closer look at how these peptides operate I see a lot of potential.
That's why when I heard about a peptide called Imunofan from a Beta Cell Project member living in Eastern Europe, my interest was piqued.
The more I looked into Imunofan - its clinical history in Soviet Russia, its applications in cancer research and immunomodulation - the more I fell in love with it.
So I've taken to outlining everything I've learned about this 6 amino acid sequence and what it can do. Let's look a bit closer at what Imunofan is, how it works, who its for and if it's something worthy of being added to our healing arsenals.
Biochemistry and Mechanism of Action
Structure and Origins: Imunofan is a synthetic hexapeptide with the amino acid sequence Arg-Asp-Lys-Val-Tyr-Arg (often noted RDKVYR). It was designed as an analog of the thymic hormone thymopoietin. This makes Imunofan closely related to the well-studied pentapeptide thymopentin (RKDVY), but with modifications (e.g. an additional C-terminal arginine) to enhance stability and activity. Imunofan is typically formulated as an arginyl-aspartyl-lysyl-valyl-tyrosyl-arginine diacetate salt (45 µg per ampoule) for injection. If you need to refresh your memory on the role of the thymus check out this article.
This structure is hydrophilic and allows Imunofan to interact with various biomolecules. Notably, Imunofan is derived from thymopoietin – a 49-amino-acid thymus hormone involved in T-cell differentiation – but is much smaller, which facilitates its use as a drug. Despite its origin as a thymic peptide, Imunofan itself is non-immunogenic and does not cause allergic reactions or antibody formation in tested models. *This is a key feature of a lot of peptides: their lack of significant side effects. Smaller, more targeted molecules limit their potential to gum up the works in other cell systems.


**Immunomodulatory Effects: Imunofan is categorized as an immunomodulatory agent – it is neither a pure immunostimulant nor an immunosuppressant. Instead, it “returns immunity indicators to the boundaries of reference values”, meaning it can upregulate deficient immune functions and downregulate excessive immune activity to restore balance. For example, in states of immune weakness, Imunofan can increase low cytokine or antibody responses, while in states of hyperimmune activation it can dampen overproduction of inflammatory mediators. This dual modulation is key to its safety and effectiveness. Mechanistically, Imunofan’s action unfolds in three phases:
Fast Phase (within hours, lasting ~2–3 days): Imunofan triggers antioxidant and detoxification pathways. It stimulates production of primary antioxidant proteins such as ceruloplasmin and lactoferrin, and increases enzymatic antioxidant activity (e.g. catalase). Consequently, there is normalization of lipid peroxidation levels and protection of cell membranes from oxidative damage. Imunofan also inhibits phospholipid breakdown and arachidonic acid release, which leads to a reduction in inflammatory eicosanoids and even a drop in blood cholesterol. At the cellular level, this phase protects tissues – for instance, during toxic liver injury, Imunofan’s antioxidant effect prevents hepatocyte death, lowering elevated liver enzymes and bilirubin.
Middle Phase (2–3 days post-dose, lasting ~1 week): Imunofan enhances innate immune functions, notably phagocytosis. It boosts the ability of macrophages and neutrophils to engulf and destroy pathogens, improving the clearance of intracellular bacteria and viruses. This corresponds to a transient immunostimulatory window where the body’s first-line defense is strengthened.
Slow Phase (7–10 days post-dose, lasting up to ~4 months): Imunofan produces longer-term immunoregulatory effects. Over weeks, it helps normalize cellular and humoral immunity parameters – for example, it can restore a healthy CD4^+/CD8^+ T-cell ratio and increase the production of specific, protective antibodies. Importantly, it tends to increase IgA levels in those with IgA deficiency (supporting mucosal immunity), without inducing IgE (allergy-related) antibodies. This indicates it doesn’t provoke allergic-type immune skewing. By this phase, Imunofan has essentially “reset” aberrant immune responses closer to normal ranges.
On a molecular level, Imunofan’s broad effects stem from its influence on immune cell signaling and gene expression. Research indicates Imunofan activates certain transcriptional programs in cells: in one transcriptomic analysis, Imunofan upregulated genes related to active DNA demethylation and epigenetic regulation in fibroblasts, and genes involved in cell migration and immune responses in stem cells. This suggests it may modulate the epigenetic status of immune cells or tissue cells to favor repair and balanced immune function. Notably, Imunofan’s action seems to be direct on cells rather than purely via inducing secondary cytokines – in cell culture, it did not massively alter cytokine secretion profiles, implying it can act within cells to alter their behavior (e.g. promote proliferation or gene expression) without necessarily causing those cells to release a cascade of inflammatory signals.
This cell-intrinsic mode of action is further supported by its demonstrated ability to stimulate proliferation of human fibroblasts and keratinocytes directly in vitro (20–50% increase in growth) with no cytotoxicity.
** This is one of the most exciting qualities about peptide use. Imunofan isn’t forcing a one-size-fits-all response; it’s acting almost like a biological whisperer, reading the body's immunological "mood" and nudging it back toward equilibrium. The risk of an unintended outcome is so low because Imunofan is enhancing the body's natural ability to self-correct, as opposed to imposing something it may not be ready or equipped for.
Immune Modulation and Cytokines: Although Imunofan itself does not dramatically force cells to secrete cytokines in isolation, it has profound effects on immune mediator balance in vivo, especially under immune challenge. For instance, a clinical study on humans undergoing diphtheria vaccination showed that the vaccine alone disturbed cytokine patterns – TNF-α production by blood cells was suppressed while IL-6 was elevated, and paradoxically serum TNF levels spiked for weeks. Pre-treatment with Imunofan normalized these cytokine responses. In other words, Imunofan prevented the abnormal post-vaccine cytokine swings: it kept pro-inflammatory TNF-α from both dropping too low in immune cells and overshooting in serum, and it tempered IL-6 elevation. By restoring a proper TNF/IL-6 balance, Imunofan potentially reduces “cytokine stress” on the body and may prevent post-vaccination inflammatory complications. More broadly, Imunofan has been reported (in earlier studies from the 1990s) to adjust cytokine profiles in various conditions – for example, lowering excessive tumor necrosis factor (TNF) and interleukin-6, or promoting beneficial cytokines like IL-2 depending on what the body needs. This flexible cytokine modulation contributes to shifting the immune system toward a balanced Th1/Th2 response and increasing regulatory control. It’s worth noting that Imunofan does not activate dendritic cells or T cells in a non-specific manner (lab tests showed it did not upregulate activation markers indiscriminately). Instead, it preserves a “resting” phenotype unless an immune challenge is present, underscoring its safety in avoiding hyperactivation.
Redox Regulation: A hallmark of Imunofan’s mechanism is its role as an “indirect antioxidant.” By inducing the production of the body’s own antioxidant proteins, Imunofan combats oxidative stress which is tightly linked to chronic inflammation. In patients with immune dysfunction, studies found deficiencies in primary antioxidants like superoxide dismutase (SOD), catalase, lactoferrin, and ceruloplasmin, accompanied by excessive lipid peroxidation and free radical damage. Imunofan corrects this by boosting those endogenous antioxidant defenses, thereby breaking the vicious cycle of oxidative stress and immune dysregulation. And if you'll remember, beta cells are notoriously deficient in these antioxidants.
Specifically, as noted above, Imunofan upregulates ceruloplasmin (a ferroxidase that safely sequesters iron and scavenges radicals) and lactoferrin (an iron-binding glycoprotein with antioxidant and anti-inflammatory properties) in the acute phase of its action. By doing so, it neutralizes reactive oxygen species and peroxides, and prevents downstream damage such as lipid peroxidation of membranes. The overall result is a reduction in inflammatory mediators and a “reset” of immune cell function from a pro-oxidative, activated state to a more regulated state. In fact, one review described Imunofan’s effect as activating the detoxification-antioxidant system which lowers the content of inflammatory mediators, normalizes cellular immunity indices, and even reduces auto-immune reactions. This redox modulation is highly relevant to diseases where chronic inflammation and oxidative stress go hand in hand.
Impact on Drug Resistance: An interesting and unique aspect of Imunofan’s mechanism is its influence on cellular transport pumps. Imunofan has been shown to inhibit the multidrug resistance (MDR) efflux pumps (such as P-glycoprotein) on cell membranes. In tumor cells, this translates to suppression of chemotherapy drug resistance, making cancer cells more susceptible to the effects of cytotoxic drugs. While the exact molecular interaction with MDR proteins is not fully elucidated, this effect has positioned Imunofan as a potential adjunct in oncology (by reversing drug resistance). It likely occurs in the slow phase of action as the peptide alters gene expression related to transporters. This MDR-inhibition, combined with its detoxifying effects, highlights that Imunofan works at the level of protein regulation and possibly post-translational modification (e.g. affecting transporter activity) to improve therapeutic outcomes.
In summary, Imunofan’s mechanism of action can be seen as a cascade of regulatory changes: it initiates antioxidant and anti-inflammatory defenses, boosts innate immune clearance, and long-term re-balances adaptive immunity and immune memory. On the molecular scale it modulates gene expression (including those involved in epigenetics and cell cycling), and on the cellular scale it calibrates cytokine release and immune cell activation state. Through these multi-level actions, Imunofan achieves a homeostatic modulation of the immune system and tissue environment rather than a one-directional immune push. This profile is particularly attractive for chronic conditions like autoimmunity, where gentle restoration of balance is needed.
Clinical Background of Imunofan
Development History: Imunofan was developed in the early 1990s in Russia during a surge of interest in immunoregulatory peptides. It was created by a team of scientists led by Prof. V. V. Lebedev at the Central Research Institute of the Russian Ministry of Health, and later produced by the enterprise “NPP BIONOKS,” founded in 1991. The peptide’s design was informed by earlier thymus extracts and peptides (like thymosin and thymopentin) but aimed to be a more potent, small synthetic molecule with broad regulatory effects. The composition and sequence of Imunofan were patented in the Russian Federation (Patent No. 2062096). By the mid-1990s, Imunofan had undergone clinical evaluation in Russia, demonstrating efficacy in various immunodeficiency and inflammatory conditions. It was among the first synthetic thymic peptide drugs to reach wide clinical use in the region. Over “almost thirty years of experience” with Imunofan, Russian clinicians accumulated a broad understanding of its applications, and it became available through the standard pharmacy network as a prescription immunomodulator. The importance of Imunofan was such that it was even labeled a “strategic product” in some Russian publications. (Indeed, a 2004 issue of a Russian intelligence agency bulletin highlighted Imunofan’s value, indicating interest beyond just the health sector.)

Regulatory Status: Imunofan gained official approval in Russia in the 1990s as an immunomodulatory drug. It has since been registered and prescribed in several post-Soviet countries. For example, it has seen medical use in Ukraine and other CIS states for immunotherapy, and there are reports of its use in Eastern Europe (anecdotal usage in places like Poland or Serbia via import channels). However, Imunofan is not approved by the US FDA or EMA as a drug; outside of its home region it remains relatively obscure and is not part of mainstream Western pharmacopoeia. In recent years, Imunofan can be obtained through specialized peptide pharmacies or as part of clinical trials, but it is typically considered an experimental or alternative therapy in Western countries. Its long track record in Russia – where it can be prescribed by immunologists or oncologists – contrasts with its virtually unknown status in North America. That said, growing interest in peptide therapeutics globally has led some clinicians (especially in integrative medicine) to take note of Imunofan for off-label use.
Original Indications: Imunofan’s initial indications were in conditions of secondary immunodeficiency. It was first used to support patients with compromised immunity – for instance, individuals with chronic infections, or those undergoing chemotherapy. Early uses included adjuvant therapy in vaccination and infectious disease prophylaxis. Imunofan was shown to enhance vaccine responses; it has been given to adults as an adjuvant to routine vaccines (e.g., against bacterial infections like diphtheria or viral infections) to ensure a stronger and more balanced immune reaction. Additionally, it was used to prevent exacerbations of chronic infections in immunocompromised hosts. By normalizing immune function, it could reduce flare-ups of diseases like chronic hepatitis or chronic brucellosis (a bacterial infection), especially when these diseases were accompanied by immune weakness.
Therapeutic Uses (Current and Past): Over time, Imunofan’s clinical use expanded impressively. It has been or is being prescribed in the following contexts (often as part of combination therapy):
Chronic Viral Infections: Imunofan is used in chronic viral hepatitis B and C to help control liver inflammation and boost antiviral immunity. It can improve the patient’s response to antiviral drugs and protect the liver via its hepatoprotective effect. Similarly, it has been used in HIV/AIDS patients – not to replace antiretrovirals, but to bolster the immune system and help fight off opportunistic infections (like CMV, herpes, Toxoplasma, Pneumocystis). Reports indicated that Imunofan co-therapy in HIV could increase CD4 counts and decrease frequency of opportunistic infections, aligning with its immune-restoring capacity.
Bacterial and Parasitic Infections: Imunofan has indications for difficult bacterial infections such as brucellosis (a chronic intracellular infection), where enhancing macrophage killing is beneficial. It has also been given in severe cases of diphtheria and even to carriers of diphtheria to help eradicate the bacterium. There is experimental use of Imunofan in parasitic diseases: for example, a study in mice with trichinellosis (parasite infection) found that adding Imunofan to a vaccine or extract therapy improved protection, though another report suggested Imunofan could interfere with certain anti-helminthic treatments. These mixed results underscore that its use in parasitic infections is still being understood. Nonetheless, Imunofan clearly can influence the immune response to pathogens and is seen as a general immune booster against chronic infections.
Oncology: Perhaps one of the most widespread uses of Imunofan in practice is as an adjunct in cancer therapy. Oncologists have used Imunofan in patients undergoing chemotherapy and radiotherapy – particularly in advanced (Stage III-IV) cancers – to improve tolerance to treatment and immune surveillance. Imunofan’s ability to restore immune parameters helps cancer patients rebound from the immune-suppressive effects of chemo/radiation. It has been noted to reduce treatment toxicity and infection rates in these patients, and as mentioned, to sensitize tumor cells to chemotherapy by blocking drug-efflux pumps. Cancers where Imunofan has been tried include lung cancer, breast cancer, melanoma, and others (often in combination with standard care). While not a stand-alone cancer drug, it is prescribed as part of comprehensive cancer care in some Russian protocols, classified under “immunotherapy” to improve outcomes and life quality. (It should be noted that formal large-scale trials in Western oncology are lacking, but Russian clinical experience over decades has built a case for its benefit in cancer patient management.)
Autoimmune and Inflammatory Diseases: Imunofan’s immunoregulatory effect has naturally led to its use in autoimmune conditions. Rheumatologists in Russia have incorporated Imunofan in difficult cases of rheumatoid arthritis, where it can help reduce inflammation and possibly modulate the aberrant immune attack on joints. Patients with severe psoriasis (an immune-mediated skin disease) have also been treated with Imunofan as part of immune correction therapy. In these diseases, Imunofan is thought to help by reducing pro-inflammatory cytokines (like TNF-α, IL-6) and increasing regulatory mechanisms, thereby alleviating symptoms. Some reports indicate that Imunofan can reduce the frequency of arthritis flare-ups or extent of psoriatic plaques, especially when conventional therapies alone are insufficient. Its use has also been explored in bronchial asthma or chronic obstructive bronchitis (“broncho-obstructive syndrome”) to mitigate excessive immune reactions in airways, and in inflammatory eye diseases such as uveitis, where immune balance is crucial.
Pediatrics: Imunofan is approved for use in children over 2 years old in certain indications. Pediatricians have used it to prevent toxic complications during chemotherapy for childhood leukemias/lymphomas. It has also been given to children with recurrent respiratory infections (to shore up immunity) and in juvenile chronic infections. One specific pediatric use is in juvenile laryngeal papillomatosis (caused by HPV) – Imunofan can be part of therapy to help the child’s immune system suppress the growth of papillomas.
This for me was a clincher for its safety claims. Very rarely do these marginal alternative medicines get clearance for children this young. I saw that as a testament to its validity as something lacking toxicity or unwarranted risks.
Adjuvant in Surgery and Wound Healing: Clinically, Imunofan has been administered to patients with severe burns (III-IV degree) and non-healing wounds as part of the management of wound sepsis and systemic inflammation. Its effects in enhancing tissue repair have also been noted anecdotally. Indeed, as discussed in research, Imunofan can promote fibroblast and keratinocyte proliferation, suggesting a role in tissue regenerative therapy. Surgeons have used it in cases of long-term ulcers or post-surgical non-healing wounds to stimulate healing. Imunofan’s inclusion in such protocols indicates that beyond immune normalization, it provides a pro-repair microenvironment (via anti-oxidative and gene-regulatory means) that can be harnessed in clinical practice.
Where It’s Prescribed Today: Currently, Imunofan remains primarily prescribed in Russia and neighboring countries. It is integrated into standard treatment guidelines for some conditions in those countries – for example, it might be listed as an optional immunotherapy for chronic hepatitis or oncology support in Russian clinical guidelines. Hospitals and clinics in the region stock Imunofan (it is available in ampoules for injection, and also as a nasal spray form for milder outpatient use). In places like Poland, Imunofan is not officially authorized as a drug, but Polish researchers have accessed it for studies, and patients sometimes obtain it through international pharmacies. In Western Europe and the US, off-label interest is growing: some integrative medicine physicians import Imunofan for patients with refractory autoimmune diseases or chronic fatigue, attracted by its long safety record and unique mechanism. Nevertheless, the use in these areas is anecdotal and not mainstream. Regulatory approval outside the former USSR has not been pursued aggressively, partly due to the need for extensive new trials.
One should note that Imunofan’s safety profile is well-established: it has very few contraindications (aside from standard ones like individual hypersensitivity). It is even considered for use in sensitive populations – for instance, it’s only contraindicated in pregnancy if there is a Rhesus immune conflict (due to its immune effects), but otherwise could be used if benefits outweigh risks. Side effects are minimal; it does not cause significant allergic reactions nor systemic toxicity at recommended doses, as evidenced by both decades of clinical use and dedicated tests (e.g., basophil activation tests showed no histamine release). This safety, combined with multi-faceted efficacy, is why Imunofan continues to be a valuable if under-recognized tool in immune-related disorders.
In summary, Imunofan’s clinical journey began in the context of immunodeficiency and has expanded to a wide array of diseases with immune involvement. Its current use spans infectious disease, oncology, autoimmunity, and regenerative medicine. While geographically limited in official status, knowledge of Imunofan is spreading, and it represents a potential addition to comprehensive therapy for conditions like type 1 diabetes, as we explore next, given its immune-balancing and tissue-protective properties.
Body Systems Impacted by Imunofan
Imunofan has systemic effects that ripple across multiple organ systems. By modulating the immune system and redox state, it indirectly or directly influences the function of various physiological systems. Here we detail its impact on key body systems and what users or patients might expect both symptomatically and mechanistically:
Immune System
As an immunomodulator, Imunofan’s primary target is the immune system. It affects virtually all arms of immunity:
Adaptive Immune Balance: Imunofan restores equilibrium between overactive and underactive immune responses. For a patient with chronic inflammation, Imunofan can reduce excessive Th1/Th17-mediated cytokines (like IFN-γ, TNF-α, IL-6) and autoantibody production, thereby alleviating autoimmune reactions. Conversely, in an immunodeficient state (low T-cell counts or poor antibody responses), it can enhance T-cell function and antibody generation. Over a course of Imunofan therapy, one might observe previously high inflammation markers (e.g. TNF, C-reactive protein) dropping toward normal, and low markers (e.g. IgG levels, CD4 counts) rising toward normal. Clinically, patients often report reduced frequency and severity of infections (due to improved immune defense) and diminished autoimmune flares (due to tempered pathological immunity). For example, rheumatoid arthritis patients might experience less joint swelling, and chronic infection patients fewer fevers.
Innate Immune Function: Imunofan bolsters innate immunity by stimulating phagocytic cells. Neutrophils and macrophages show increased microbicidal activity after Imunofan use. This means an improved ability to clear bacteria, fungi, and viruses in early infection stages. Symptomatically, a patient might notice that wounds or infections clear faster. Imunofan also maintains a healthy activity of natural killer (NK) cells and does not hyperactivate them in absence of a threat – this controlled enhancement helps in surveilling for viruses or tumor cells while avoiding NK-mediated tissue damage.
Regulatory/Anti-Inflammatory Pathways: An important immune effect is the support of regulatory pathways. There is evidence that Imunofan can increase levels of IL-4 and IL-10 in situations where anti-inflammatory response is needed (though data is mostly from animal models and indirect observations). These cytokines promote a regulatory (Th2/Treg) bias which counteracts aggressive Th1 responses. Imunofan’s lack of effect on IgE and possible boosting of IgA also reflect a tilt away from allergic inflammation toward protective mucosal immunity. Patients with conditions like allergic asthma might find that Imunofan does not worsen allergies and may even reduce atopic inflammation indirectly.
So much of our identification of autoimmunity in the West today relies on reading into the Th1-Th2 balance. Those with autoimmune conditions, like T1D, are Th1 dominant, and thus lack the "off" side of the immune response.
Thymus and Lymphoid Organs: Given its thymic origins, Imunofan interestingly has trophic effects on the thymus gland. Studies in rats showed that Imunofan delays age-related thymic involution, preserving thymic structure and output of new T cells. This suggests that in humans, Imunofan might help maintain thymus function in older or chronically ill individuals – essentially acting as a thymus support, ensuring continued education of T cells. Imunofan’s developer (Lebedev) reported that chronic use led to positive shifts in thymocyte populations. Users might not “feel” this directly, but over long term it could mean a more robust naive T-cell pool and better immune vigilance.
Immune Surveillance and Cancer Defense: By virtue of normalizing immunity, Imunofan can enhance the body’s natural surveillance against malignant cells. Its stimulation of cytotoxic T lymphocytes (CTLs) and NK cells (when needed) could improve the detection and elimination of nascent tumor cells. While this is hard to measure symptomatically, one tangible effect seen in patients is improved outcomes when Imunofan is used alongside cancer therapies (e.g., slower tumor progression or improved blood counts during chemotherapy). Imunofan does not itself cause tumor shrinkage, but by reducing immunosuppression and oxidative stress, it creates an internal environment less friendly to cancer growth.
Overall, users of Imunofan often experience an improvement in immune-related symptoms: fewer infections, more energy (as chronic inflammation abates), and if they have an autoimmune disease, possibly a reduction in pain or inflammation severity. Importantly, because Imunofan recalibrates rather than simply boosts immunity, it has a gentle side effect profile – one does not see the severe flu-like reactions that can occur with pure interferon treatments, for example.
Nervous System
Imunofan’s direct impacts on the nervous system are less pronounced than on the immune system, but there are several indirect influences:
Neuro-Immune Interactions: The reduction in pro-inflammatory cytokines like TNF-α and IL-6 can significantly benefit the nervous system. These cytokines, when chronically elevated, contribute to sickness behavior (fatigue, malaise) and can cross the blood-brain barrier to induce neuroinflammation. By lowering systemic inflammation, Imunofan may alleviate such symptoms. Patients with chronic inflammatory diseases often report improved energy levels and cognitive clarity after a course of Imunofan, likely because their cytokine milieu is normalized. In conditions like multiple sclerosis or other neuroinflammatory disorders (though not formally studied with Imunofan yet), the peptide’s immune balancing could hypothetically reduce autoimmune attack frequency on neural tissue.
Stress Axis and Endocrine Effects: Immune modulation by Imunofan can affect the hypothalamic-pituitary-adrenal (HPA) axis. There is evidence that immunostimulation therapies lead to feedback changes in the pituitary gland. In an experimental model of immunostimulation, researchers observed ultrastructural changes in pituitary thyrotropic cells (which produce TSH), hinting that immune signals (or immune modulators like Imunofan) can influence pituitary hormone production. While detailed endocrine studies in humans are lacking, Imunofan might indirectly improve HPA-axis regulation by reducing the chronic stress of inflammation. Some patients have noted better sleep and mood stabilization on Imunofan, which could be due to reduced cytokine interference with neurotransmitters.
Neuroprotective Potential: Through its antioxidant boosting, Imunofan may protect neurons from oxidative damage. Neurodegenerative processes are often exacerbated by oxidative stress. By elevating catalase, SOD, and related enzymes in peripheral and possibly central cells, Imunofan could lower the burden of reactive oxygen species that can damage neural tissues. For example, lactoferrin (which Imunofan increases) has known neuroprotective effects in models of neurodegeneration. Although Imunofan is not primarily a neurological drug, these effects raise the possibility that it could be beneficial in conditions like diabetic neuropathy or chemo-induced neuropathy by creating a more anti-oxidative systemic environment.
Safety on Nervous Tissue: It’s important that Imunofan has shown no neurotoxic effects. In vitro tests confirmed that Imunofan is not toxic to primary neural cells at a wide range of concentrations. It doesn’t impede neural cell viability or neurite outgrowth. Clinically, there have been no reports of neurotoxicity or cognitive adverse effects; on the contrary, as mentioned, patients often feel a subjective improvement in well-being. Unlike some immune therapies (e.g., high-dose IL-2 or interferons) that cause significant CNS side effects (depression, etc.), Imunofan’s gentle modulation tends to avoid this.
In sum, while Imunofan is not a neurologic medication per se, its immune normalization provides a more favorable environment for the nervous system. Patients might experience indirect benefits such as improved mood, less brain fog, and potentially improved nerve function, especially in ailments where inflammation and oxidative stress impinge on the nervous system.
Hepatic and Detoxification Systems (Liver)
The liver is both a target and a beneficiary of Imunofan’s actions:
Hepatoprotective Effects: Imunofan has a documented hepatoprotective effect in toxic and viral liver injury. By boosting antioxidant defenses (ceruloplasmin, catalase) in the liver, it helps neutralize free radicals generated by toxins or hepatitis viruses. It also stabilizes hepatocyte membranes by curbing lipid peroxidation. In acute liver stress (such as chemotherapy-induced hepatotoxicity or viral hepatitis flare), Imunofan has been shown to reduce liver enzyme levels (ALT, AST) and lower bilirubin faster than standard care alone. This suggests it mitigates liver cell destruction. Patients with hepatitis who take Imunofan often show improved liver function tests and report reduction in symptoms like fatigue or jaundice.
Antioxidant Enzyme Induction: The liver is a major source of circulating antioxidant proteins, and Imunofan stimulates the liver’s production of ceruloplasmin, a copper-containing enzyme that also carries out ferroxidase activity (converting Fe^2+ to Fe^3+ and facilitating iron binding to transferrin). Higher ceruloplasmin means better control of free iron in the blood (which otherwise can catalyze free radicals). It also indicates an acute phase response that is protective. Along with ceruloplasmin, the increase in catalase activity in the liver helps decompose hydrogen peroxide, reducing oxidative injury. The net effect is a liver environment less prone to inflammatory damage. Patients with fatty liver disease or chronic hepatitis might see a slow improvement in liver inflammation markers over an Imunofan course.
Detoxification and MDR: Imunofan aids the liver’s detox role by both preventing damage (so the liver can do its job) and by modulating drug transporter activity. The liver’s expression of P-glycoprotein and other transporters can be down-regulated by Imunofan, potentially improving the retention of therapeutic drugs. For example, in a cancer patient, Imunofan might allow chemotherapy drugs to remain longer in liver tumor cells rather than being pumped out, thereby enhancing efficacy. For someone on multiple medications, Imunofan could theoretically alter drug metabolism/excretion profiles slightly (though in practice no adverse drug interactions are well documented, likely because the effect is mainly within pathological cells like tumor cells).
Symptomatic Impact: Patients with chronic liver conditions who use Imunofan often feel less “toxic” – they may have better appetite, less nausea, and more stable weight. These subjective improvements align with objective findings like reduced cytokines (e.g. IL-1, TNF) which are often elevated in liver diseases and cause systemic malaise. Additionally, by lowering cholesterol levels modestly (via reduced hepatic synthesis of cholesterol from arachidonic acid pathways), Imunofan might have a slight beneficial effect on lipid profiles, although this is a secondary outcome.
In summary, Imunofan supports the liver by creating an antioxidant-rich, anti-inflammatory milieu, allowing for better detoxification and resilience against insults. This is particularly relevant in Type 1 Diabetes if there is any concomitant fatty liver or if frequent glycemic swings cause oxidative stress that the liver must manage.
Gastrointestinal System (Gut)
The gut, while not a primary target of Imunofan, can be influenced by the peptide’s systemic actions:
Mucosal Immunity: Imunofan’s increase of IgA production is beneficial for the gut’s immune defense. IgA is the antibody that patrols mucosal surfaces (intestine, respiratory tract) and helps maintain a healthy microbiome balance by neutralizing pathogens. Individuals with low IgA (including some type 1 diabetics who have selective IgA deficiency or celiac disease co-morbidity) could experience improved gut immunity from Imunofan. This might manifest as fewer gastrointestinal infections or a reduction in gut inflammation. For instance, anecdotal reports suggest that chronic diarrhea in immunocompromised patients improved when on Imunofan, likely due to restored IgA levels and better pathogen control.
Anti-Inflammatory in the Gut: In inflammatory bowel conditions, Imunofan could in theory help by the same mechanisms as elsewhere – reducing inflammatory mediator overflow. A study on rats with gastric mucosal injury showed that Imunofan (thymohexin) protected the stomach lining, largely by inhibiting inducible nitric oxide synthase (iNOS) and reducing oxidative damage in the gastric mucosa. iNOS is often upregulated in gut inflammation (like in Crohn’s disease or ulcerative colitis), leading to excess NO and peroxynitrite that harm tissues. By inhibiting this, Imunofan demonstrated a cytoprotective effect on the GI tract. Extrapolating to humans, patients with gastritis or ulcers might see improved healing with Imunofan’s addition. Indeed, Imunofan has been used to promote healing of peptic ulcers and reduce GI side effects of NSAIDs in some settings, given its mucosal protective qualities.
Microbiome and Infection: The gut is home to a vast microbiome and is often where systemic infections can take root (think of Salmonella, or translocation of bacteria in sepsis). By boosting phagocytic activity and local immune surveillance, Imunofan can help prevent translocation of bacteria from the gut in critically ill patients. In surgical patients with abdominal infections or cholecystopancreatitis (combined gallbladder and pancreatic infection/inflammation), Imunofan was included in therapy to reduce septic complications. This suggests it helps contain infection spread from the GI source. While not a direct antibiotic, Imunofan’s immune support in the gut could mean less severe infections and faster clearance. Patients might experience, for example, that an episode of bacterial gastroenteritis resolves more swiftly or with less systemic upset if Imunofan is on board (though formal studies would be needed to confirm this).
Gut Healing and Motility: There is emerging interest in peptides for gut healing (e.g., BPC-157 is known for this); Imunofan might also contribute to gut tissue repair indirectly. Its general pro-repair effect (fibroblast stimulation) could facilitate healing of intestinal lesions. Additionally, by decreasing inflammation, it could improve gut motility (since inflammation can cause dysmotility or neuropathy in the gut). Patients with inflammatory conditions sometimes report normalization of bowel habits when their systemic inflammation is addressed.
Overall, Imunofan’s impact on the GI system is supportive – a healthier immune environment leads to a healthier gut. While not specific for gastrointestinal disorders, Imunofan helps maintain mucosal immunity and reduces the collateral damage of inflammation in the digestive tract. For a type 1 diabetic, who might have an associated autoimmune gut issue (like autoimmune gastritis or celiac sprue), Imunofan could potentially ease those by the same immune balancing.
Endocrine Pancreas (Beta Cells and Metabolic Effects)
Of special interest is Imunofan’s potential impact on the endocrine pancreas, which is highly relevant for type 1 diabetes (T1D):
Modulating Autoimmunity in Pancreas: T1D is caused by an autoimmune attack on pancreatic β-cells. Imunofan’s ability to reduce autoimmune reactions suggests it could lessen this attack. By normalizing T-cell function and promoting regulatory mechanisms, Imunofan might slow the destruction of remaining β-cells in early or even established T1D. In principle, Imunofan could shift the balance from a destructive insulitis (inflammatory infiltration of islets) to a more benign or resolving inflammation. For example, it might reduce levels of interferon-gamma and IL-17 secreting T cells that target islets, while enhancing regulatory T cells that protect islets. Though direct studies in T1D models are not yet published, Imunofan has been shown to cut down pathological immune responses in other autoimmune models, so a similar effect in the pancreatic islets is conceivable. Clinically, if Imunofan were given to a person with recent-onset T1D, one might hope to see a preservation of C-peptide (indicating some continued insulin production) over time, or a decrease in markers of β-cell autoimmunity (such as islet autoantibody titers or T cell reactivity). These are hypotheses that warrant testing.
Reducing Beta-Cell Stress: Even after autoimmunity has killed most β-cells, the remaining ones (or transplanted new ones) often struggle under inflammatory stress. Cytokines like IL-1β and TNF-α, produced in the islets by infiltrating immune cells, cause β-cell dysfunction and apoptosis. Imunofan’s systemic lowering of these cytokines can relieve the inflammatory stress on β-cells. Additionally, oxidative stress in islets – which can be high due to autoimmune and hyperglycemic conditions – would be countered by Imunofan’s antioxidant boost. Iron dysregulation has been implicated in β-cell toxicity; excess iron catalyzes free radical formation leading to β-cell apoptosis. Imunofan increases lactoferrin, which chelates free iron, and ceruloplasmin, which facilitates safe iron transport. This means Imunofan could help sequester any loose iron in inflamed islets, preventing it from fueling oxidative destruction. In essence, Imunofan may create a more hospitable environment for β-cells by dialing down the “toxic inflammation” in the pancreas. Patients might not directly feel this at first, but over months it could translate to better glucose control (as β-cells work more efficiently) or reduced insulin requirements if some endogenous function is preserved.
Metabolic and Glycemic Effects: Imunofan is not a hypoglycemic agent, but by addressing systemic inflammation, it can improve insulin sensitivity and metabolic parameters. Chronic inflammation is known to induce insulin resistance; cytokines like TNF disrupt insulin signaling. By lowering such cytokines, Imunofan may enhance insulin sensitivity in peripheral tissues. There’s also evidence linking inflammation to dysregulated gluconeogenesis in the liver – so Imunofan could reduce inappropriate glucose output by calming inflammatory signals to the liver. Some patients (especially type 2 diabetics or those with metabolic syndrome overlap) have noted minor improvements in fasting glucose and cholesterol levels when on Imunofan therapy, likely due to these systemic improvements.
In T1D specifically, any preserved C-peptide or reduced inflammation might help mitigate blood sugar volatility. However, it’s important to clarify that Imunofan is not a replacement for insulin; its role would be adjunctive – potentially reducing the autoimmune drive and preserving what beta-cell mass is left, which could result in a longer “honeymoon period” in new-onset T1D or at least a reduction in insulin dose needed by the patient if some endogenous production remains.
Pancreatic Regeneration Avenues: Emerging strategies for T1D include beta-cell regeneration or replacement (via stem cells, etc.). Imunofan might play a synergistic role here. For any regenerative therapy to succeed, the inflammatory milieu must be controlled; otherwise new beta cells are destroyed as well. Imunofan could serve as an immune-conditioning agent to support beta-cell regeneration strategies – for instance, if one were attempting to convert alpha cells to beta cells or deliver stem-cell-derived islets, Imunofan might improve engraftment by dampening autoimmunity and inflammation during the process. Furthermore, Imunofan’s effect on gene expression (like upregulating the demethylation enzymes and even pluripotency-related factors like OCT4 in some cells) hints that it might encourage a pro-regenerative state. This is speculative, but intriguing: a peptide that modulates the immune system and epigenome could facilitate the pancreas’s own attempt to regenerate insulin-producing cells once immune attack is mitigated.
Symptomatically, a person with type 1 diabetes taking Imunofan might notice over time that they have fewer inflammatory symptoms (for instance, less joint pain or other autoimmune phenomena that sometimes accompany T1D), and potentially a stabilization of their insulin requirements. If Imunofan indeed helps preserve beta-cell function, one outcome could be fewer and less severe hypoglycemic or hyperglycemic swings because the body retains some capacity to buffer glucose changes. It could also theoretically reduce complications driven by inflammation (such as slowing progression of diabetic neuropathy or retinopathy, which are exacerbated by inflammatory pathways).
In summary, Imunofan’s impact on the endocrine pancreas is protective and modulatory. It tackles the immune-mediated destruction and stress that afflict pancreatic islets in T1D. While it is not a standalone cure for diabetes, in a comprehensive healing strategy Imunofan could serve as the “immune shield,” creating conditions under which pancreatic healing measures (like beta-cell regeneration, immunotherapy, or transplantation) can be more effective. The ultimate hope is that by protecting β-cells from the immune system’s friendly fire, Imunofan might help extend their longevity and function in diabetic patients.
Iron Metabolism, Oxidative Stress, and Inflammatory Links in T1D
One of the intriguing aspects of Imunofan is how it interfaces with iron metabolism and oxidative stress, which are increasingly recognized in the pathology of chronic inflammatory diseases and possibly type 1 diabetes. Here we explore these connections:
Iron Dysregulation in Inflammation: During chronic inflammation (as seen in autoimmunity or persistent infections), the body often sequesters iron – a phenomenon underlying the “anemia of chronic disease.” Key proteins like lactoferrin and ceruloplasmin, produced mainly in neutrophils and the liver respectively, are part of this response: they bind and redistribute iron to limit its availability to pathogens and to reduce iron-catalyzed free radical production. In many autoimmune conditions, however, iron metabolism becomes imbalanced. There may be elevated ferritin (an acute phase reactant storing iron) but functional iron deficiency in tissues, causing stress. In T1D, some researchers have posited that local iron accumulation in islets or high oxidative load contributes to β-cell damage. In fact, in rare “bronze diabetes” (hemochromatosis), massive iron overload in the pancreas causes diabetes by directly killing β-cells. While T1D is not caused by iron overload, micro-level dysregulation of iron and oxidative stress in inflamed islets could be a cofactor that accelerates β-cell loss.
Imunofan’s Role in Iron and Antioxidant Balance: Imunofan is notable for upregulating lactoferrin and ceruloplasmin shortly after administration. Lactoferrin is a potent iron-binding protein; it chelates free iron in the bloodstream and tissues, denying fuel to harmful bacteria and also preventing iron from participating in Fenton chemistry that generates hydroxyl radicals. Ceruloplasmin, on the other hand, oxidizes Fe^2+ to Fe^3+, facilitating its loading onto transferrin and incorporation into safe storage or usage pathways. By boosting these proteins, Imunofan reduces the pool of free reactive iron at sites of inflammation. In doing so, it cuts down on the generation of highly reactive free radicals (like •OH).
The significance for T1D is that Imunofan can mitigate iron-driven oxidative toxicity in pancreatic islets. During the autoimmune attack on islets, activated immune cells release not only cytokines but also reactive oxygen and nitrogen species. If iron is present, it exacerbates this oxidative assault. Imunofan’s lactoferrin surge would bind any loose iron in the islet microenvironment, and its catalase induction would break down excess hydrogen peroxide. This one-two punch greatly diminishes oxidative stress. A reduction in oxidative stress is crucial because oxidative damage to β-cells can cause their apoptosis and also make them appear abnormal, potentially even more antigenic (oxidative modifications of proteins can create neo-epitopes). Thus, Imunofan may help interrupt a vicious cycle in T1D: inflammation → oxidative stress → β-cell damage → release of β-cell antigens → more autoimmunity. By lowering inflammation and oxidative stress simultaneously, it spares β-cells and gives a chance for immune tolerance to reset.
Lactoferrin, Ceruloplasmin, and Diabetes: There is some evidence outside of Imunofan research that supports the importance of these factors in metabolic disease. Lactoferrin has been studied as a therapeutic supplement; for instance, oral lactoferrin was found to reduce oxidative stress and inflammation in diabetic rodents, improving pancreatic insulin secretion and insulin sensitivity. It’s also been noted that low circulating lactoferrin correlates with chronic inflammation and insulin resistance in humans. This implies that raising lactoferrin (as Imunofan does endogenously) could have anti-diabetic effects. Similarly, ceruloplasmin is known to increase in inflammation, but if it’s not sufficiently induced, iron can accumulate in tissues and cause harm. By ensuring a robust ceruloplasmin response, Imunofan helps keep iron in circulation and out of sensitive places like pancreatic islets.
Furthermore, Imunofan’s activation of the antioxidant system extends to enzymes like superoxide dismutase (SOD) and glutathione peroxidase, as observed with other thymic peptides. While those specific enzymes weren’t mentioned in the Imunofan product literature, the conceptual overlap suggests Imunofan-treated individuals likely experience a rise in SOD and glutathione activity as well, given the tight regulation of antioxidant networks. This comprehensive antioxidant upregulation means a reduction in lipid peroxides and oxidized DNA in tissues.
Chronic Inflammation and Beta-Cell Toxicity: Chronic inflammation in T1D not only kills β-cells but can also cause a state of functional suppression of β-cells due to nitrosative stress (from excess nitric oxide) and ER stress. Imunofan’s inhibition of iNOS (as seen in gastric mucosa models) likely applies to pancreatitis or islet inflammation contexts too – it would reduce harmful NO levels. Moreover, by decreasing systemic TNF-α and IL-1β, Imunofan removes key instigators of β-cell apoptosis. There is a known pathway where IL-1β + IFN-γ induce β-cell death via NF-κB and STAT1 signaling; Imunofan’s cytokine modulation could dampen these pathways. In essence,
Imunofan attacks the inflammation-oxidation duo on multiple fronts: it lowers inflammatory cytokines, raises anti-inflammatory cytokines, chelates iron, neutralizes peroxides, and improves the antioxidant enzyme milieu. This concerted action addresses many of the hypothesized contributors to β-cell toxicity in diabetes.
From a theoretical standpoint relevant to comprehensive diabetes care, one could liken Imunofan to a “reset button” for the oxidative-inflammatory state. When used in someone with type 1 diabetes, Imunofan might help shift the body from a pro-inflammatory, pro-oxidant state (which not only damages β-cells but also contributes to insulin resistance and vascular complications) to an anti-inflammatory, antioxidant state. This could reduce systemic markers like malondialdehyde (a lipid peroxidation product) and CRP (an inflammation marker), which are often elevated in poorly controlled diabetes and linked to complications. Lowering these could translate to less endothelial damage (hence possibly slowing development of diabetic complications such as nephropathy or retinopathy which have inflammatory components).
Speculative Emerging Link – Ferroxidation and Autoimmunity: Some emerging hypotheses suggest that improper ferroxidase activity (e.g., low ceruloplasmin or related proteins) might trigger autoimmunity by allowing reactive iron to modify self-proteins. Imunofan’s ability to boost ceruloplasmin could therefore indirectly reduce the emergence of neoantigens that drive autoimmunity. Although this is speculative in T1D, it’s an example of how far-reaching the iron-immune connection can be, and Imunofan sits right at that intersection by restoring the anti-oxidant, iron-binding branch of immunity.
In conclusion, Imunofan’s modulation of iron metabolism and oxidative stress is highly relevant to the inflammation seen in T1D. By inducing lactoferrin, ceruloplasmin, and antioxidant enzymes, Imunofan removes one of the silent killers of beta cells: oxidative radical damage. This not only protects existing beta cells but also reduces overall inflammation (since oxidized molecules often perpetuate immune responses). The tight integration of these effects positions Imunofan as a unique therapy that can address a root contributor to chronic inflammatory damage, complementing therapies that address the immune cells or blood sugar directly. This synergy of immune and oxidative control is what makes Imunofan a promising component of a holistic T1D treatment strategy focused on healing and preservation.
Comparison with Other Immunomodulatory Peptides
Imunofan is one among several bioactive peptides that modulate the immune system and promote healing. To put its properties in context, we compare it here to a few other known immunomodulatory peptides – Thymosin alpha-1, LL-37, and BPC-157 – especially regarding inflammation, immune balance, and tissue regeneration:
Imunofan vs. Thymosin Alpha-1 (Tα1)
Thymosin alpha-1 is a 28-amino-acid peptide originally isolated from the thymus (and now synthesized), widely studied as an immune-activating agent. It shares thymic origins with Imunofan but differs in size and specific function. Key points of comparison:
Mechanism of Action: Tα1 primarily enhances T-cell mediated immunity and the function of dendritic cells. It is known to act as a Toll-like receptor 2 and 9 agonist on dendritic cells, thereby promoting antigen presentation and a robust adaptive immune response. This leads to increased production of Th1 cytokines (like IL-2, IFN-γ) and activation of cytotoxic T lymphocytes. Imunofan, in contrast, doesn’t directly agonize pattern-recognition receptors as far as known; its immunomodulation is more downstream, adjusting immune cell output and oxidative environment. Both peptides modulate and normalize T-lymphocyte populations, but Tα1 is often characterized as more of an immune enhancer (especially in immune-deficient states), whereas Imunofan is an immune balancer (up or down as needed).
Cytokine Profile: Tα1 tends to promote a Th1 bias and has been shown to increase IL-2 and IFN-γ production in various contexts, improving cell-mediated immunity (for example, in chronic hepatitis B). Imunofan can also enhance a Th1 response if deficient, but it is equally capable of reducing an excessive Th1/Th17 response. Interestingly, Tα1 has some anti-inflammatory aspects too: studies have found it can increase IL-10 and regulate the immune response to prevent over-inflammation, particularly by promoting regulatory T cells in certain disease models. Imunofan similarly avoids overshooting inflammation and can elevate IL-4/IL-10 when needed. So in terms of immune balance, both peptides ultimately aim to restore homeostasis, but Tα1 achieves this by boosting the immune system’s competence (especially in fighting infections or cancer), whereas Imunofan achieves it by damping pathology and filling gaps.
Antioxidant Effects: Tα1 has been discovered to have antioxidant gene effects as well – it can upregulate SOD, catalase, and glutathione peroxidase, thereby reducing oxidative tissue damage. In fact, Tα1’s antioxidant properties are cited as beneficial in conditions like chronic pancreatitis or hepatitis where oxidative stress is high. This is quite analogous to Imunofan’s induction of antioxidant defenses (catalase, etc.). The difference might be in magnitude or timing: Imunofan induces these very quickly (within hours) as part of its “fast phase”, whereas Tα1 might have a more gradual effect via gene induction. Nonetheless, both peptides combat oxidative stress associated with chronic inflammation, which is a notable convergence in their mechanism.
Clinical Use: Thymosin α1 (brand name Zadaxin in some countries) is an approved drug in many places for treating conditions like hepatitis B and C, and it’s used in some cancers and as an adjuvant for vaccines (e.g., it’s an FDA-approved orphan drug for malignant melanoma and is used in combination therapies for HIV, etc.). Imunofan, as discussed, is approved mainly in Russia for a wide array of similar indications (chronic infections, cancer adjuvant, etc.). Both have good safety profiles. Tα1 typically requires subcutaneous injection 2-3 times a week in clinical use, whereas Imunofan might be given in short daily courses with long-lasting effects (up to months of effect).
Summary: Tα1 and Imunofan are complementary in concept – one can imagine Tα1 as the peptide you use to “restore immune strength” and Imunofan as the peptide to “restore immune balance.” For instance, in a patient with chronic viral infection, Tα1 directly increases the ability to clear the virus by activating T cells, while Imunofan would ensure that activation doesn’t cause collateral damage and that the immune system returns to a stable baseline after clearing the virus. In practice, Imunofan’s more pronounced effect on innate antioxidant responses and its MDR-reversal in cancer are unique features where Tα1 has less data. Conversely, Tα1’s direct TLR-mediated mechanism gives it a role as a vaccine adjuvant and anti-infective that Imunofan (lacking known receptor-binding) had to earn through experiential use rather than clear molecular targeting. Both could be considered for autoimmune diabetes interventions, but Tα1 might risk pushing autoimmunity if not carefully balanced, whereas Imunofan inherently would try to quell autoimmunity.
Imunofan vs. LL-37
LL-37 is a human cathelicidin antimicrobial peptide (37 amino acids long) that serves double duty as a broad-spectrum antibiotic and an immune modulator. While not used clinically as a systemic therapy (it’s an endogenous peptide), it’s relevant as an immunomodulatory molecule:
Antimicrobial and Immunomodulatory Actions: LL-37 directly kills bacteria, enveloped viruses, and fungi by disrupting their membranes. But beyond that, it has complex immunomodulatory roles. It can promote inflammation by recruiting immune cells and inducing chemokine production, and it can also act as an anti-inflammatory agent in certain contexts. For example, LL-37 is known to neutralize lipopolysaccharide (LPS), thereby blocking an overzealous inflammatory response to gram-negative bacteria. It can also inhibit the AIM2 inflammasome and suppress cytokines like TNF-α, IL-12, and IFN-γ when they are excessive. Imunofan, comparably, doesn’t have direct microbe-killing ability, but it helps the immune system fight microbes. Both Imunofan and LL-37 can be said to help the host fight infections while modulating inflammation; however, LL-37 is part of the innate immune “immediate response,” whereas Imunofan orchestrates a later regulatory response.
Role in Autoimmunity: LL-37 has been implicated in autoimmunity in a paradoxical way – it’s found at high levels in diseases like psoriasis and lupus. In psoriasis, LL-37 forms complexes with self-DNA, which can trigger plasmacytoid dendritic cells and cause interferon production (an autoimmune stimulus). Imunofan, in contrast, has generally been observed to reduce autoimmunity. Where LL-37 might inadvertently fuel autoimmune signaling by acting as a “danger signal,” Imunofan’s effect is to reduce danger signaling (by lowering cell damage and inflammatory mediators). So, therapeutically, one would not give LL-37 to an autoimmune patient (it might exacerbate things), whereas Imunofan is given to calm autoimmunity.
Tissue Healing: Both peptides have roles in tissue repair. LL-37 has been shown to promote wound re-epithelialization, angiogenesis, and modulation of matrix metalloproteinases. It helps in wound healing by attracting neutrophils and macrophages to clear debris and by directly stimulating growth factors in some cases. Imunofan also promotes wound healing, as evidenced by fibroblast and keratinocyte proliferation in experiments, but it does so likely via different pathways (e.g., gene expression changes, reduced chronic inflammation that otherwise impairs healing). In a chronic wound scenario, LL-37 would act early to prevent infection and kick-start inflammation, whereas Imunofan would act later to ensure that inflammation resolves and that cells can proliferate and remodel tissue properly.
Use in Therapy: LL-37 itself is not yet a drug (though analogs are being explored for infections and wound healing). Imunofan, as a drug, harnesses some of the benefits we attribute to innate peptides like LL-37 (controlling infection, modulating inflammation), but in a way that can be administered systemically with control. For instance, one could consider Imunofan in someone with a non-healing diabetic foot ulcer; it might not directly kill bacteria like LL-37 would, but by boosting the patient’s immunity and reducing systemic inflammation (which can impair wound healing), it could improve outcomes alongside antibiotics.
In summary, LL-37 is like the acute-phase infantry of immunity, while Imunofan is more like the peacekeeping and rebuilding force. LL-37's immunomodulation is context-dependent – it can incite or quiet inflammation – whereas Imunofan is deliberately designed to quiet abnormal inflammation and support recovery. Both emphasize the point that immune modulation is not one-directional; timing and context matter. Imunofan’s advantage is that it’s been tuned (through design and clinical feedback) to typically push toward resolution and balance, whereas LL-37 as a natural peptide will do whatever the local environment biases it to do (sometimes promoting, sometimes resolving inflammation).
Imunofan vs. BPC-157
BPC-157 (Body Protection Compound-157) is a 15-amino-acid peptide derived from a protein found in gastric juice. It has gained attention for its powerful tissue healing and anti-inflammatory properties. Comparison points:
Tissue Regeneration: BPC-157 is most famous for accelerating healing of ulcers, tendon injuries, ligaments, bone fractures, and even nerve damage. It promotes angiogenesis (formation of new blood vessels), collagen deposition, and granulation tissue formation. Imunofan also aids tissue repair but more by modulating the environment (inflammation/oxidation) and a modest direct proliferative effect on skin cells. BPC-157 seems to have a more direct growth-factor-like effect on tissues – it upregulates genes involved in cell survival and growth in wounded tissue, as noted in rat wound models. If one imagines a trauma or ulcer, BPC-157 is the peptide that dramatically speeds the physical repair processes, whereas Imunofan ensures the immune aspect of healing (preventing chronic inflammation or infection) is optimized. They could be synergistic: one rebuilding tissue scaffolding (BPC-157) and the other controlling the “biochemical climate” for healing (Imunofan).
Anti-Inflammatory Effects: BPC-157 does exhibit notable anti-inflammatory effects across multiple organ systems. It has been shown to reduce pro-inflammatory cytokine levels in models of IBD (inflammatory bowel disease) and arthritis, for instance. It also protects the gut and liver from NSAID damage, partly by quelling inflammation. Imunofan’s anti-inflammatory effects are systemic and subtler in onset (a regulatory effect rather than direct inhibition). BPC-157 can directly bind and neutralize certain inflammatory mediators or affect local signaling (for example, it interacts with the NO system, balancing nitric oxide effects, which can reduce edema and pain). Imunofan, as described, works through the immune system’s own regulatory pathways to reduce inflammation. The outcomes (decreased swelling, pain, inflammatory cell infiltration) may be similar, but BPC-157 might achieve these faster in an acute injury, whereas Imunofan would shine in a chronic inflammatory state.
Immune System: Unlike Imunofan and Tα1, BPC-157 is not primarily known as an immune modulator. It doesn’t significantly alter immune cell subsets or antibody production; its effects on the immune system are secondary to its repair functions (for example, by healing the gut lining, it indirectly reduces antigenic load and immune activation; by reducing inflammation, it spares immune cells from constant activation). Imunofan clearly engages with immune regulation (phagocytes, T-cells, etc.), something BPC-157 does much less of. Thus, for autoimmune conditions, Imunofan would be more directly useful than BPC-157. For mechanical injuries or organ damage, BPC-157 is very potent, whereas Imunofan would be supportive.
Usage and Safety: BPC-157, like Imunofan, is used off-label in many places (BPC-157 is not officially approved as a drug, but is widely available as a research compound). Both have excellent safety profiles in studies, with BPC-157 showing no toxicity even at high doses in animal tests. BPC-157 is typically given orally or by injection and has localized effects especially on the gut when taken orally (because it remains active in the GI tract). Imunofan is usually injected (or nasal spray) to achieve systemic distribution. For a patient, taking BPC-157 might result in rapid pain relief and healing of, say, a tendon injury, with less noticeable impact on things like infection rates or allergy symptoms. Taking Imunofan, the patient might notice improvements in chronic symptomatology (like less fatigue, fewer colds), but it won’t regrow cartilage or close an ulcer as visibly as BPC-157 can.
In summary, BPC-157 is a regenerative powerhouse with moderate immune-calming abilities, while Imunofan is an immune regulator with moderate regenerative abilities. In a condition like type 1 diabetes, BPC-157 might help repair gut or vascular damage associated with diabetes or possibly protect the pancreas from some physical stress, but it wouldn’t address the autoimmune cause; Imunofan would address the autoimmune/inflammatory cause, but not by itself regenerate islets. This again underscores the idea of a combination therapy approach, where different peptides play different roles.
Shared and Unique Features
All these peptides – Imunofan, Thymosin α1, LL-37, BPC-157 – share a common theme of immunomodulation and inflammation control. Each, however, targets different aspects:
Imunofan: Broad immune normalization + antioxidant boost.
Thymosin α1: Immune stimulation (especially cellular immunity and antiviral defense) + some immune restoration in deficient states.
LL-37: Innate immune defense (antimicrobial) + context-dependent immune signaling, bridging innate and adaptive responses.
BPC-157: Tissue protection and regeneration + localized anti-inflammatory action.
One notable point is that none of these peptides is immunosuppressive in the traditional sense – they do not wipe out or blunt the immune system like corticosteroids or calcineurin inhibitors do. Instead, they modulate the quality of the immune response. This makes them attractive for chronic conditions where you want to avoid shutting down immunity (which would invite infections) but you need to rein in harmful inflammation or promote healing.
From an inflammation standpoint:
Thymosin α1 and LL-37 can both induce and reduce inflammation, but generally in therapy Tα1 is used to reduce chronic inflammation by treating the underlying cause (e.g., clearing infection or restoring balance), and LL-37 is still experimental.
Imunofan consistently tends to reduce chronic inflammation (by multiple mechanisms described).
BPC-157 tends to reduce acute and chronic inflammation at injury sites.
From an immune balance standpoint:
Imunofan and Tα1 both aim to restore immune homeostasis – Tα1 by filling in for thymus function (enhancing immunity where it is low), Imunofan by an adaptive see-saw correction (down if too high, up if too low).
LL-37 is part of natural balance – too much LL-37 can be pathological (psoriasis), but the right amount helps maintain immune equilibrium against microbes.
BPC-157 isn’t directly about immune balance, but by healing tissues (especially gut barrier), it indirectly prevents aberrant immune activation (since a healthy gut prevents excessive immune exposure to microbes and food antigens).
From a tissue regeneration perspective:
BPC-157 is at the forefront, used for musculoskeletal injuries and gut lining repair.
Imunofan has a moderate effect – e.g., 8–36% improvement in wound closure in mice models – so it’s contributory but not as dramatic as BPC.
Thymosin α1 is not typically noted for regeneration, except it may help recovery of the thymus and hematopoiesis.
LL-37 helps clear damaged tissue and initiate repair but is not known for, say, regrowing tissue on its own.
Thus, Imunofan stands out by covering a broad spectrum (immune, antioxidant, anti-inflammatory, some healing) but at a moderate level each, whereas these other peptides are more specialized in their high-impact domains. For a disease like type 1 diabetes which involves autoimmunity (Imunofan, Tα1 would be relevant), chronic inflammation and potentially microbial triggers (Imunofan, LL-37 relevant), and tissue injury (BPC-157 relevant if we consider islet or gut or vascular damage), one can see that a multi-pronged approach might be needed. Imunofan could be a central component to handle the immune/inflammatory side, potentially used in concert with others (if that were to be explored in the future).
Expanded Use Cases and Emerging Applications of Imunofan
Beyond the contexts already discussed, Imunofan has shown promise or has been experimented with in a variety of other diseases and conditions. Its broad mechanism lends itself to any scenario involving immune dysfunction, chronic inflammation, or oxidative stress. Below are some notable expanded use cases and areas of exploration:
Autoimmune Diseases: We touched on rheumatoid arthritis and psoriasis, but Imunofan has been tried in other autoimmune-like conditions. For instance, there are anecdotal uses in systemic lupus erythematosus (SLE) where the goal is to reduce flares by normalizing immune response. Similarly, in multiple sclerosis (MS) (an immune-mediated CNS disease), peptides like thymosin and Imunofan have theoretical benefit in shifting the immune profile toward less inflammation. While direct studies on Imunofan in MS or SLE are scarce in the literature, its efficacy in reducing auto-antibody production and T-cell overactivation could be harnessed here. Clinicians in Russia have occasionally reported using Imunofan in refractory autoimmune cases as an adjunct to standard therapy, noting reductions in ESR (erythrocyte sedimentation rate) and other inflammation markers.
Chronic Fatigue Syndrome (CFS) / ME and Fibromyalgia: These complex syndromes often involve dysregulated immune responses and chronic inflammation at low levels. Imunofan might help by correcting subtle immune imbalances. Indeed, some patients with CFS who took immunomodulators like Imunofan reported improvements in energy and cognitive function. While this is anecdotal, it aligns with the idea that restoring a normal cytokine milieu (reducing elevated inflammatory cytokines that can cause fatigue) can ameliorate symptoms. Imunofan’s long-lasting action (up to 4 months from a short course) is particularly convenient for chronic syndromes, potentially providing prolonged relief between doses.
Allergies and Asthma: Imunofan is not an antihistamine or typical allergy medication, but by modulating the immune system, it can impact allergic conditions. The fact that Imunofan does not increase IgE and even slightly suppresses IgE-driven responses means it could be useful in atopic conditions. In practice, some physicians have used Imunofan in atopic dermatitis (eczema) or allergic asthma with the aim of reducing the Th2-skewed hyper-responsiveness. For example, in allergic asthma, Imunofan might help by increasing IFN-γ (which counter-regulates Th2) and ensuring that IgE levels don’t rise. Russian literature suggests Imunofan helped reduce the severity of bronchial asthma attacks when used over time (likely by controlling the underlying inflammation rather than as a rescue medication).
Viral Epidemics (e.g., COVID-19): During the COVID-19 pandemic, Russia and neighboring countries experimented with various immunomodulators. While the spotlight was on drugs like interferon and thymosin α1, Imunofan also came up in discussions as a way to bolster immunity in vulnerable individuals and possibly prevent cytokine storm. Its profile of enhancing antibody responses to vaccines and controlling excessive cytokines could theoretically be valuable in viral infections with hyperinflammation phases. There were some reports (not large trials) of Imunofan being given to COVID-19 patients or as prophylaxis to healthcare workers to improve their resilience, with claims that it reduced incidence or aided recovery. These remain anecdotal, but they open an emerging application: using Imunofan or similar peptides in acute severe infections to modulate the immune response – boosting the early phase (to fight the virus) and mitigating the late hyperinflammatory phase (to prevent ARDS or organ damage). More formal studies would be needed to confirm any benefit in this area.
Immunosenescence and Aging: As mentioned, Imunofan helps delay thymic involution and maintain immune parameters in the elderly. This makes it a candidate for anti-aging or geroprotective strategies. In older adults, the immune system tends to become both weaker (prone to infections, poor vaccine responses) and more inflammatory (a phenomenon called “inflammaging”). Imunofan addresses both: it can improve vaccine responses and resistance to infections (hence could be given prior to flu season, etc.), and it reduces chronic low-grade inflammation by enhancing antioxidant systems. One could envision Imunofan being used in geriatric medicine to improve overall immune health and possibly reduce the incidence of age-related diseases that have an immune component (like certain cancers or Alzheimer’s, which has an inflammatory aspect). Indeed, because Imunofan was considered a “strategic product,” it was speculated that it might be used to keep aging populations healthier or even for military personnel to maintain performance under stress.
Cancer Adjunct Therapy (Expanded): Beyond its use during chemo, Imunofan may have other roles in oncology. For example, it has been explored in melanoma immunotherapy in combination with cancer vaccines or checkpoint inhibitors, to try to increase tumor antigen presentation and normalize the immune response in the tumor microenvironment. Another niche use is in preventing cancer recurrence: after curative treatment, some oncologists have considered using Imunofan in a maintenance phase to keep the immune system actively surveying for residual cancer cells. Given its low toxicity, it could be given periodically for years to help the immune system remain vigilant. It’s also noteworthy that Imunofan was used in veterinary oncology (e.g., in dogs with transmissible venereal tumor or cats with leukemia virus) to boost their immunity and outcomes.
Chronic Infection Control: Outside of acute infections, Imunofan has been used in diseases like tuberculosis (TB) and Lyme disease. In TB, especially multi-drug-resistant TB, the immune system is often subverted. Russian doctors added Imunofan to TB treatment regimens to try to improve the immune clearance of Mycobacterium tuberculosis, seeing some improvements in sputum conversion rates. In chronic Lyme or other persistent infections, where immune evasion is an issue, Imunofan could similarly assist in rallying the immune system to suppress the pathogen better after antibiotics have reduced the load. These are emerging or investigational uses that stem from the peptide’s general immune normalization capability.
Parasitic and Tropical Diseases: As referenced, Imunofan was tested in helminth infections (like trichinosis). It’s also been mentioned in context of malaria or leishmaniasis (diseases where Th1 response is needed but over-inflammation causes pathology). The idea is to use Imunofan to support the correct immune response while avoiding excessive inflammation. In one study on an organophosphate toxin exposure, Imunofan corrected the skewed production of TNF and other cytokines, highlighting that even in toxin-induced inflammation, it has a role. Extrapolating that, for any illness where a toxin or parasite triggers immune chaos, Imunofan might help restore order.
Metabolic and Cardiovascular Diseases: Chronic low-level inflammation is a driver of atherosclerosis, insulin resistance, and other metabolic disorders. While Imunofan is not a primary therapy for these, reducing inflammation and oxidative stress can benefit these conditions. For example, in patients with type 2 diabetes or metabolic syndrome, Imunofan might improve their profile by lowering inflammatory cytokines that contribute to insulin resistance. Also, lactoferrin (boosted by Imunofan) has been found to have beneficial effects on adiposity and metabolism. There’s an interesting study where higher lactoferrin predicted lower risk of heart disease in diabetics, suggesting that Imunofan’s induction of lactoferrin might even be cardio-protective in the long term. These potential uses are quite exploratory, but as our understanding of chronic inflammation’s role in diseases broadens, Imunofan or similar immunomodulators might find a place in preventive medicine for metabolic and vascular health.
Gaps in the Literature and Speculations: While the above paints an optimistic picture, it’s important to note gaps:
Lack of Large-Scale Trials: Most of Imunofan’s reported benefits come from small studies, open-label experiences, or non-English literature (Russian studies that may not have large sample sizes or rigorous controls by Western standards). For conditions like type 1 diabetes, no clinical trial data exists yet – its use would be founded on mechanistic rationale and cross-applying data from other autoimmune conditions. Rigorous trials are needed to validate Imunofan’s efficacy in new indications and to quantify outcomes (e.g., preserving C-peptide in new-onset T1D, or reducing insulin dose, etc.).
Mechanistic Uncertainties: We still don’t know Imunofan’s direct molecular target. Is there a specific receptor on immune cells it binds to (like Tα1 with TLR)? The manufacturer information suggests it was modeled on thymopoietin’s active site, which historically was thought to interact with T cells to induce differentiation. Thymopentin (the shorter fragment) is known to restore T-cell rosette formation, implying a receptor on T cells. Imunofan’s slight sequence alteration might have been to increase stability, but the receptor could be the same thymopoietin receptor (which remains not well-characterized). Understanding this could help tailor its use or combine it smartly with other therapies. Also, the extent of its epigenetic effect needs more study – the wound healing study found no consistent transcriptional pattern, meaning Imunofan’s gene effects might depend on cell context or initial state (which fits its modulatory nature).
Optimal Dosing and Regimens: The typical Imunofan regimen in Russia is an injection every day or every other day for 5-10 doses, then a break of several months. Is that optimal for all conditions? Could smaller but continuous dosing (e.g., via nasal spray daily for longer) maintain steadier immune regulation? We don’t know for sure. If applying it to T1D, one might consider continuous low-dose therapy vs periodic re-dosing – these strategies would need exploration. Overdosing doesn’t seem to be a risk in toxicity, but could an overdose tilt the immune balance too far in some direction? Thus far, Imunofan hasn’t shown immune suppression even at high doses, which is reassuring.
I recently purchased Imunofan and did the 10 day treatment: 45mcg in solution, 1x per day for 10 straight days.
Combination Therapy Considerations: Another gap is how Imunofan interacts with other treatments. In T1D, if used alongside conventional immunotherapies (like teplizumab, an anti-CD3 antibody, or low-dose IL-2 to boost Tregs), would it enhance or interfere? No data exists yet, but such combos could be powerful: Imunofan providing broad support while a targeted therapy provides specific intervention. Similarly, in cancer, combining Imunofan with checkpoint inhibitors (like anti-PD-1) could be interesting – Imunofan might improve the overall immune health while checkpoint inhibitors unleash specific anti-tumor T cells. These possibilities remain speculative but suggest a direction for future research.
I used imunofan while also using semaglutide (0.25-0.5mg weekly), syrian rue capsules (~50mg harmine) and 1x verapamil tablet (120mg extended released) with no adverse effects.
Emerging Hypotheses: Finally, some emerging hypotheses around Imunofan include its effect on the microbiome (since it modulates immune factors that shape microbiota) and on stem cell niches (given some hints of OCT4 upregulation in fibroblasts, could Imunofan be nudging certain cells to a more progenitor-like state to aid repair?). In context of T1D, one could hypothesize that Imunofan might help bone marrow stem cells mobilize or help progenitor cells in the pancreas to survive the inflammatory environment longer – these are very early ideas without direct evidence.
In conclusion of the expanded uses: Imunofan’s versatility as an immunomodulator has led to its trial in many conditions – from infections to autoimmunity to adjunctive cancer care, and even theoretical use in chronic metabolic diseases. Its core effects of correcting immune deviations and reducing oxidative stress provide a unifying explanation for these diverse applications. While many of these uses are promising, they also underscore the need for more formal research. For type 1 diabetes specifically, Imunofan represents a compelling piece of a holistic strategy: it could address the autoimmune attack and inflammatory milieu that are not tackled by insulin therapy alone. When combined with antigen-specific therapies (like tolerogenic vaccines) or regenerative approaches, an agent like Imunofan might significantly tilt the odds in favor of pancreatic islet survival and even functional improvement. This synergy of old and new interventions – using a peptide with decades of clinical use (Imunofan) in concert with cutting-edge diabetes treatments – exemplifies the innovative, comprehensive thinking needed to tackle complex diseases like T1D from multiple angles.
Hopefully you come away from this article with a better picture of how Imunofan may be able to serve the T1D collective. A thymus-derived peptide designed to enhance the body's innate ability to modulate our naturally immunity. To reduce excess inflammation, cytokine release and autoimmunity while simultaneously re-invigorating the self-regulating capabilities of the antioxidants and regulatory enzymes needed to re-establish immune balance.
It’s especially fascinating because this regulatory flexibility — upregulating where there’s weakness, calming when there’s chaos — is more like how the thymus and other intelligent network hubs operate. It’s like Imunofan reinstates the body's innate sense of self-regulation, which in chronic disease tends to get buried under layers of inflammation, immune confusion, and oxidative noise.
There’s something very poetic about a compound that doesn’t override the body, but instead reminds it of balance. And in the context of type 1 diabetes — where destruction often arises not from sheer aggression but from miscommunication, overload, and metabolic desperation — a gentle conductor like Imunofan might be one of the missing pieces.
It also opens up a broader question: How many chronic conditions are simply the result of a lost rhythm — where the body still knows what to do, but the signals are scrambled? Peptides like Imunofan aren’t necessarily “cures,” but they might just be the translators between dysregulation and restoration.
I see this as a perfect adjunct to enhance existing efforts to preserve, protect and proliferate existing beta cell mass. From what we've gathered it can be done safely, with next to no residual complications or side effects.
References:
Goldstein G. et al. (1979). Science 204:1309-1310 – Identification of thymopoietin’s active pentapeptide (thymopentin)
Nasadyuk C. & Sklyarov A. (2013). Regul. Pept. 180:50-57 – Thymohexin (Imunofan) showed gastric mucosal protection via iNOS inhibition and reduced oxidative damage.
Pukhalsky A.L. et al. (1996). Mediators Inflamm. 5(6):429-433 – Imunofan pretreatment normalized TNF-α and IL-6 production after diphtheria vaccination.
Lebedev V.V. (2004). Vestn Ross Akad Med Nauk (2):34-40 – Imunofan as an indirect antioxidant increases endogenous antioxidants (SOD, catalase, lactoferrin, ceruloplasmin), lowers inflammation mediators, and corrects cell immunity, reducing autoimmune reactions.
Imunofan Product Monograph (Peptide Products, 2020) – Pharmacology of Imunofan: immunoregulatory effects, phases of action, lactoferrin/ceruloplasmin induction, clinical indications (chronic infections, oncology, autoimmune diseases).
Sawicka J. et al. (2020). Molecules 25(12):2884 – Imunofan (RDKVYR) promoted wound healing, stimulated fibroblast/keratinocyte proliferation, induced genes for DNA demethylation and cell migration, and showed no cytotoxicity or allergy in vitro.
Dominari A. et al. (2020). World J. Virol. 9(5):67-78 – Thymosin α1 comprehensive review: immune enhancement via TLR-2/9 on dendritic cells, normalization of T-cell counts, improved antioxidant enzyme activity, and clinical uses in Hepatitis, HIV, cancer.
Zhang Y. et al. (2020). Int. J. Mol. Sci. 21(5):1636 – LL-37 review: dual roles in inflammation, can promote chemokines and also inhibit inflammasomes and cytokines (IFN-γ, TNF-α, IL-4, IL-12) depending on context.
Seo S. et al. (2018). J. Dent. Anesth. Pain Med. 18(5):287-294 – BPC-157 in incisional pain model: exhibited anti-inflammatory and wound-healing effects in multiple tissues.
Kouzmina E. et al. (2019). Russ. Immunol. J. 23(2):158-166 – (In Russian) Imunofan in immunosenescence: delayed thymus aging and improved vaccine responses in elderly (cited by manufacturer).


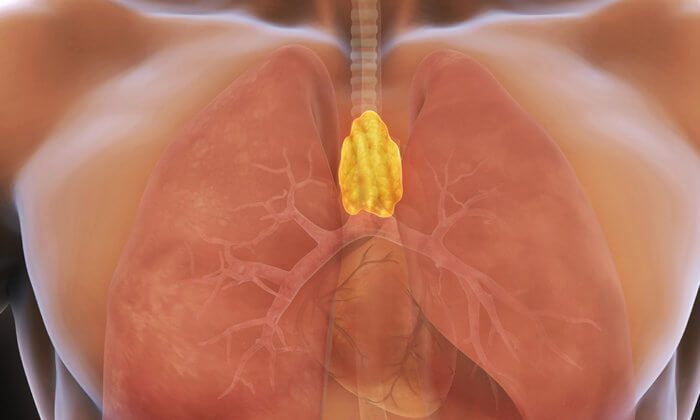
Comments